Posted on : Apr.14,2019 19:36 KST
 |
|
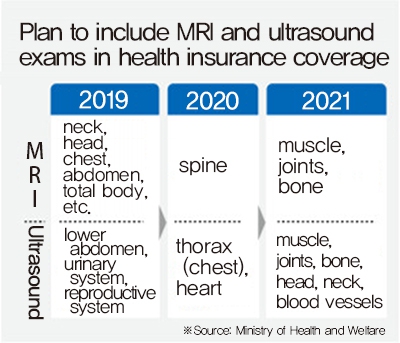
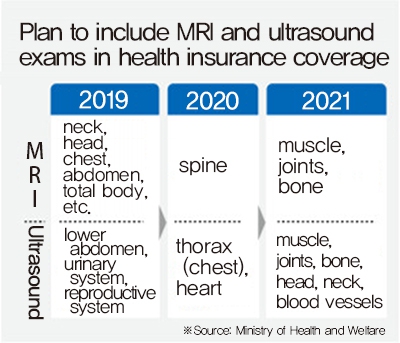
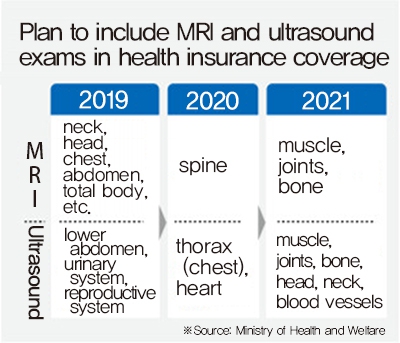
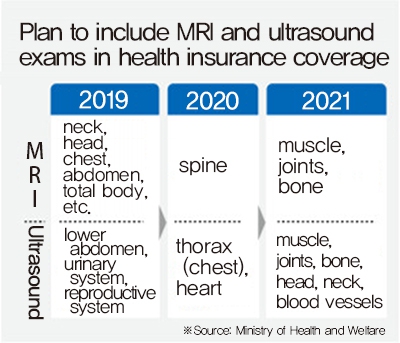
Plan to include MRI and ultrasound exams in health insurance coverage
|
Health insurance coverage to expand to include MRI and ultrasound exams
 |
|
Plan to include MRI and ultrasound exams in health insurance coverage
|
The South Korean government plans to spend around 6 trillion won (US$5.26 billion) over the next five years to reduce the financial burden for treatment of subfertility and serious illnesses in small children. The measures come in addition to the plan for “Moon-care,” an expansion of health insurance coverage for procedures such as magnetic resonance imaging (MRI) and ultrasound that carry a large financial burden for patients. Announced for the first time on Apr. 10, the comprehensive health insurance plan is formulated every five years according to the National Health Insurance Act for the purposes of sound health insurance implementation.
Announced on Apr. 10 by the Ministry of Health and Welfare (MOHW), the 1st National Health Insurance Comprehensive Plan (2019–2023) includes an expansion in health insurance guarantees for small children and subfertile couples as of this year, which joins the “health insurance security reinforcement plan” announced by President Moon Jae-in in August 2017. The existing reinforcement plan has been referred to by the nickname “Mooncare,” with a decision previously made to expand the scope of health insurance coverage to include procedures such as MRI and ultrasound examinations that were previously paid for entirely by patients.
The plan includes a pilot program this year in which home healthcare teams consisting of physicians, nurses, physical therapists, and occupational therapists visit the homes of pediatric patients with severe conditions to provide healthcare services. The house calls are expected to help in alleviating difficulties in cases involving pediatric patients with severe conditions, who often require frequent hospitalization and/or ongoing outpatient treatment. MOHW also plans to reduce the amount paid for outpatient treatment of small children as of January this year, lowering the cost from 21–42% of outpatient treatment costs to 5–20% (depending on hospital size) for infants under one year of age and from 10% to 5% for prematurely born infants under 36 months.
In the case of subfertility treatment, the ministry is to remove the current age limit of 44 years and add two to three additional health insurance coverage allowances for in vitro fertilization and artificial fertilization procedures.
The scope of health insurance coverage for MRI examinations is also set to expand, with the inclusion of spinal examinations as of next year and muscle, bone, and joint examinations as of 2021. Health insurance coverage for ultrasound examinations is also to be expanded to include chest and heart examinations next year and muscle/bone/joint, face/neck, and blood vessel examinations at a later date. Hospital room coverage is to be expanded as well, including an effort to apply health insurance to one-person rooms for dying patients. With health insurance coverage currently extended for two- to three-person rooms at tertiary and general hospitals but not for one-person rooms, MOHW determined that health insurance coverage should also be provided for the hospitalization of dying patients and those with contagious conditions in separate one-person rooms. At present, health insurance coverage is provided for a maximum of four days for a single-person room at a hospice organization exclusively for terminal cancer patients.
Increasing efficiency of healthcare systems
In addition to reinforcing health insurance security, the plan also includes measures to increase the efficiency of healthcare service usage. The aim is to ensure suitable treatment while reducing needless medical costs associated with patients visiting large hospitals for minor conditions or facing repeated hospitalization due to inadequate care outside the hospital. In particular, the plan is to encourage patients with conditions such as hypertension and diabetes that require continued management to receive treatment from neighborhood clinics and regular physicians rather than large hospitals, and to reduce unnecessary hospitalization by introducing visiting healthcare services for patients who have mobility issues.
The minimum age for the senior citizen outpatient fixed cost system – through which patients pay only a set amount for treatment at neighborhood clinics – is to be raised to 70 years from its current 65. Currently, seniors aged 65 and older pay costs of 1,500 won (US$1.32) for total treatment expenses of 15,000 won (US$13.17) or less; 10% for expenses between 15,000 and 20,000 won (US$17.56); 20% for expenses between 20,000 and 25,000 won (US$21.95); and 30% for expenses of 25,000 won or more.
“There are issues with surplus treatment, where hospitals of all scales and functions are in competition in cases where patients are unclear which hospital they should go to depending on how sick they are,” explained Oh Geon-ho, who chairs the steering committee for the group A Welfare State for the People by the People.
“Policies to rationalize the system of healthcare usage by patients represent a very important issue,” Oh said.
Some are criticizing the plan as a step backward from full coverage for previously uncovered treatments, which is seen as key to reducing medical costs.
“There was no clear reference here to ‘full coverage for uncovered treatment,’ which was a key policy in Mooncare,” said Woo Seok-gyun, policy committee chair for the Korean Federation of Medical Activist Groups for Health Rights.
“If the uncovered treatments remain in place, the medical system will just create new uncovered treatments, so there are limits to how much security can be increased even when we’re spending huge amounts of money on health insurance,” Woo observed.
Another question is whether the medical community can be expected to cooperate with policies to increase the efficiency of healthcare usage. Between 2016 and 2018, the government and healthcare providers joined for 14 meetings of a “healthcare provision system improvement consultative group” with the aim of rationalizing the healthcare usage system by clearly distinguishing the roles of hospitals and clinics, but the group concluded its activities early last year without producing any results. The Korean Medical Association has currently called off dialogue with the South Korean government as it calls for an increase in permissible medical charges.
By Kim Yang-joong, medical correspondent, and Park Hyun-jung, staff reporter
Please direct comments or questions to [english@hani.co.kr]